

Ovodonation gives women who cannot have children the opportunity to gestate an embryo on their own, from the eggs of a donor and the sperm of the receiving couple, if it is available, with the option of using the IVI semen bank if not.



Egg donation is an assisted reproductive treatment which involves an in vitro fertilisation (IVF) with eggs from a donor. Thanks to this technique, women who cannot use their own eggs due to various reasons, can still get pregnant. Donor eggs are fertilised with the partner´s or donor´s sperm if necessary and the selected embryo is transferred into the uterus of the patient. As such, oocyte donation makes the miracle of life possible for women who would not be able to have children any other way.
Egg donation can be performed with a sperm sample from a donor or the partner. This treatment is recommended for:
Our egg donation patients become pregnant after an average of 2 cycles. If you are undergoing egg donation treatment, in the first cycle, you have an 83% chance of getting pregnant (using all the embryos obtained in that cycle, but in different transfers), reaching 99% on the third attempt.
|
* Pregnancy rate after 3 cycles. Each cycle includes the first fresh embryo transfer and subsequent transfers of all embryos generated and cryopreserved in that cycle. |
* Each cycle includes the first fresh embryo transfer and subsequent transfers of all embryos generated and cryopreserved in that cycle. |
|
* Pregnancy rate after 3 cycles. Each cycle includes the first fresh embryo transfer and subsequent transfers of all embryos generated and cryopreserved in that cycle. |
|
* Each cycle includes the first fresh embryo transfer and subsequent transfers of all embryos generated and cryopreserved in that cycle. |
There are two different types of egg donation treatment at IVI. Our specialists at the clinic can advise you on the differences between the two, allowing you to decide the best one for you:
In Spain, egg donation is regulated by Law 14/2006 on Assisted Human Reproductive techniques, which establishes that there must not be any ties between the donor and the recipient, thus making sure donation is anonymous and confidential.
This anonymity works both ways, that is, the donor will never know if her eggs resulted in a baby being born nor its identity, and the mother and the baby will never have information about the donor, apart from the physical characteristics and information relevant to pregnancy monitoring.
Furthermore, the Spanish regulations state that donation is voluntary and altruistic, and as such, the donors receive no payment for it. However, financial compensation for physical discomforts, travel and labour expenses derived from the donation is contemplated within the legal framework, and it varies between €800 and €1000. In this manner, the Spanish legal framework ensures that no donation is commercial in nature or profit-driven.
Additionally, the Royal Decree – Law 9/2014 defines the quality and safety standards for donating eggs, their procurement, processing and distribution. The European law on traceability and safety of donated samples finds its expression in this norm in Spain. For this purpose, the Ministry of Health, Social Services and Equality created a platform called SIRHA, which provides the necessary tools to enforce the law.
Spain is a world leader in donations, also in the area of organs and transplants. Our donors, asked about their incentives, driven by solidarity and empathy all mention the need to help other women to become mothers.
Egg donor selection at IVI
Our donors play a crucial role in helping the patients make their dreams come true. That is why at IVI we make sure they receive the highest possible level of health care and that both our patients and donors are always given a central focus during each and every treatment.
To become a member of the egg donation programme at IVI, the donors must undergo a medical and psychological assessment. A thorough gynaecological examination is given as well, which will rule out the presence of irregularities of the reproductive organs and help us study the ovaries to predict the donor´s response to medication and the potential number of eggs.
The absence of transmissible diseases such as HIV, hepatitis and syphilis will be confirmed, and the blood group and Rh factor will also be checked. Finally, a genetic screening will be performed, including karyotype analysis, which gives us information about the chromosomes and CGT, which reduces the risk of transmitting more than 600 diseases. That way, our donors receive extremely valuable information about their fertility, their state of health and their potential to become mothers, which can be of help while planning to become mothers themselves.
Only those candidates who meet all the requirements and are completely prepared to go through the process and ready for the responsibility of being a donor, are accepted. As of today, this means that only one in three women who visit IVI and are willing to donate eggs actually get to donate.
IVI, one of the largest frozen egg banks
Thanks to the gamete donation programme, IVI has one of the largest egg banks in the world. This means we have a great variety of physical characteristics (phenotypes) at our disposal and that we can allocate the right eggs quickly, even when dealing with rare blood types. This way our patients do not have to sign up for long waiting lists to start the treatment with the best guarantees.
In the UK all donors must be between the ages of 18 and 35, fit and healthy, and have no history in the family of inherited diseases or genetic disorders. All egg donation treatment has to be non-anonymous. This is a requirement by the HFEA, the regulatory body of human reproduction in the United Kingdom. Under UK law, once the child reaches the age of 18 they will be able to contact their donor if they so wish. However, it is important to note that the parents have no legal obligation to tell the child how they have been conceived and the donor has no legal rights or responsibilities of the child once it is born.
The identity of the donor will be provided to the child, not the parent. However, when choosing the donor, as a minimum the parents will have been provided with some information about the physical appearance, for example, their height, eye colour and hair colour etc. Also, many of our donors include a short bio including their hobbies and how they would describe themselves, as well as writing a goodwill message to any children born using their donation.
There are two different types of non-anonymous donation in the UK. Regardless of which treatment the patient chooses, the HFEA deem it necessary for all parties to attend a minimum number of counselling sessions. In these sessions, our counsellors will discuss all the implications involved when it comes to an egg donation treatment in the UK.
Donor from egg bank
These gametes will have been donated by a woman who has no connection to the recipient and who has chosen to donate her eggs purely out of goodwill. The women will have only been allowed to donate if they meet the criteria set by the HFEA, this includes the correct BMI, age and medical history.
Known donor
Patients may choose to use a known donor, which means using the eggs from a friend or relative. There are restrictions when using this method to ensure the eggs do not share the same DNA as any of the recipients and the donor will still need to meet the criteria set by the HFEA to participate.
To learn more about donation in the UK and the egg donation journey, you can visit our IVI UK website.

1 blastocyst

2 blastocysts

Baby at home or 100% money back guarantee
1 blastocyst

2 blastocysts

Baby at home or 100% money back guarantee
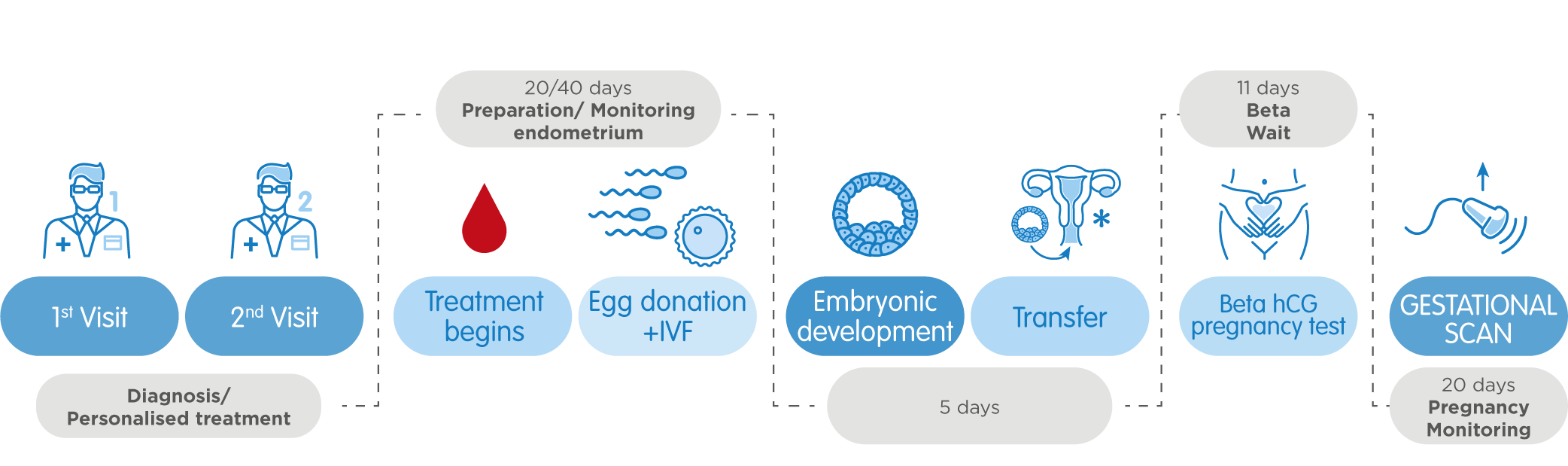
Your first visit at one of our clinics is always the first step. Our fertility experts give a personalised diagnosis and a recommendation for the treatment that best adapts to their needs. During the consultation, they analyse the patient´s medical record and all the reports relative to previous treatments carried out, if applicable. Moreover, this appointment includes a complete gynaecological examination, as well as sperm analysis in the case of heterosexual couples and the sperm sample can be frozen and stored for subsequent fertilisation.
IVI´s patients can count on Perfect Match 360° technology for the egg donation process, an innovative system that guarantees choosing the most suitable donor that includes:
This allows for taking into consideration not only physical characteristics, such as eye colour, height, blood type and Rh factor compatibility. IVI Biometric Scan takes also facial resemblance into account, backed by a software able to evaluate it on a scale from 1 to 100. Last but not least, during the selection process all our donors undergo a Compatibility Genetic Test (CGT) which enables detecting the presence of genes likely to cause up to 600 genetic diseases.
Fertilisation of the donor´s egg and the partner´s or the donor´s sperm takes place in a laboratory. At the same time, back in their home country, the patient takes fertility medication for 10 days to prepare her uterus in order to, maximise the chances of embryo implantation. This stimulation will be monitored at all times by our medical team, who supervises its correct evolution by with both ultrasound scans and blood test results.
Once in Spain, our experts will perform a transfer, introducing the best embryo into the women´s uterus by inserting a cannula, which helps access the perfect spot for the implantation. The procedure is painless, requires no anaesthesia and having rested for a couple minutes, the patient may resume everyday activity and travel back home on the very same day.
11 days after the transfer, the patient will take a blood pregnancy test. If the result is positive, 20 days later the gynaecologist will perform a control ultrasound scan on the basis on which IVI will discharge you, and you will be able to go on to monitor the pregnancy with your doctor or midwife.