



In vitro fertilisation is a complex assisted reproductive treatment. It involves joining an egg with sperm in the laboratory –in vitro– in order to obtain good-quality embryos, which once transferred to the mother’s uterus lead to a pregnancy.
To perform the procedure, it is necessary for the patient to undergo controlled hormonal stimulation to procure her eggs, which will later be fertilised in vitro in the laboratory and monitored for a few days whilst they develop. One of these embryos will then be transferred back to the womb and the rest will be frozen for future use.
In vitro fertilisation can be carried out with the sperm from the donor or the partner and it makes fertilisation easier when there are factors hindering the process. This treatment is recommended for:
At IVI, the chances of getting pregnant increase in each cycle. With your own eggs, in the first cycle, you have a 74% chance of getting pregnant (using all the embryos obtained in that cycle, but in different transfers), reaching 97% in the third cycle.
|
*Pregnancy rate after 3 cycles. Each cycle includes the first fresh embryo transfer and subsequent transfers of all embryos generated and cryopreserved in that cycle. |
*Each cycle includes the first fresh embryo transfer and subsequent transfers of all embryos generated and cryopreserved in that cycle. |
|
*Pregnancy rate after 3 cycles. Each cycle includes the first fresh embryo transfer and subsequent transfers of all embryos generated and cryopreserved in that cycle. |
|
*Each cycle includes the first fresh embryo transfer and subsequent transfers of all embryos generated and cryopreserved in that cycle. |
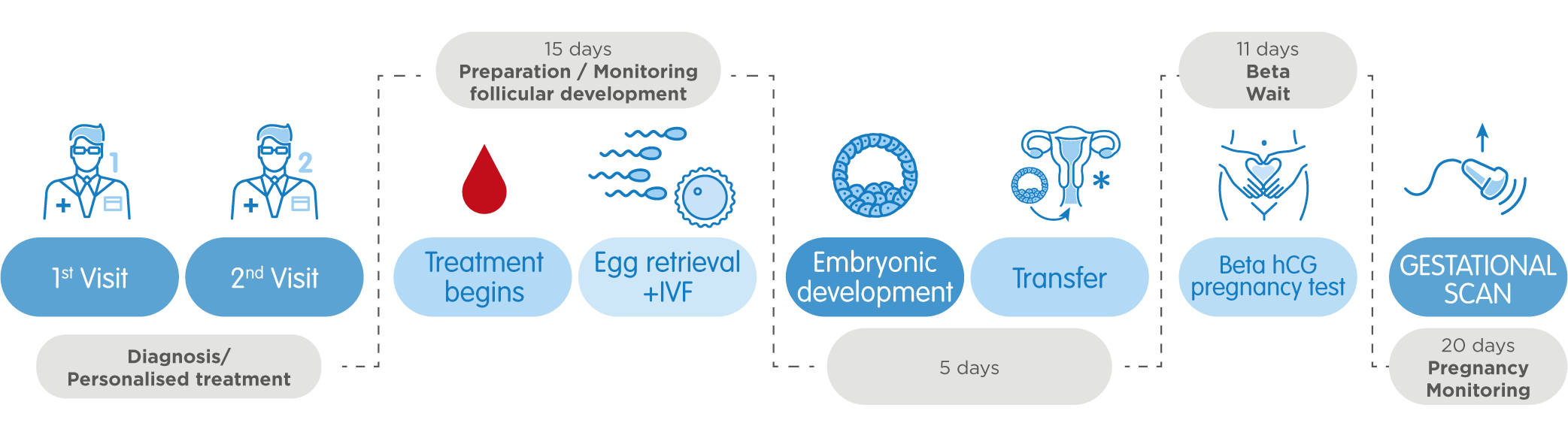
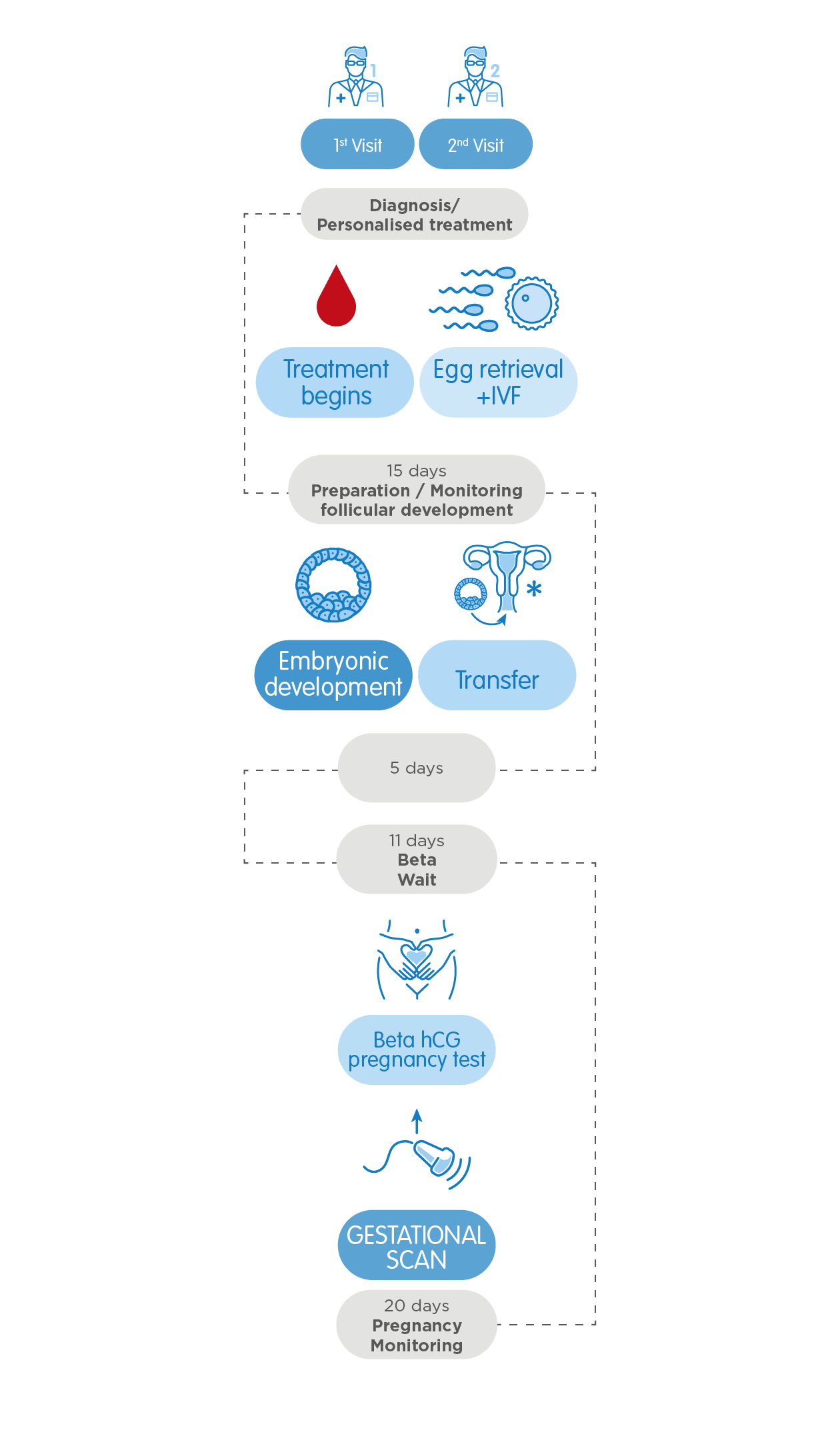
An in vitro fertilisation treatment begins with your first visit to an IVI clinic, during which our specialists diagnose the patient, analysing their medical record and all the reports relative to previous treatments carried out in Spain or elsewhere, if applicable. Moreover, this appointment includes a complete gynaecological examination, as well as sperm analysis if the partner´s sperm is to be used. By means of this personalised diagnosis, IVI makes sure their patients receive a recommendation for the treatment that best adapts to their needs.
Once back home, ovarian stimulation begins and it consists in daily injections that the patient may administer herself, if she wishes. A woman produces only one egg in each natural menstrual cycle but this 15-25 day hormonal treatment ensures the development of multiple thanks to the induction of multifollicular growth. The eggs will later be fertilised and become embryos, classified in accordance with their quality. Normally one will be transferred into the patient´s uterus and the rest will be frozen for future use. Your gynaecologist will do various ultrasound scans (3 or 4) and blood tests throughout the process to monitor how the stimulation evolves and once the follicles have reached an adequate number and size, a dose of the hCG hormone will be administered to induce oocyte maturation. 36 hours later, an oocyte retrieval will be scheduled at your IVI clinic.
It is a simple procedure, which lasts about 15-20 minutes and is carried out in an operating theatre under sedation so as not to feel any discomfort. To perform the retrieval, we access the ovaries through the vaginal cavity and puncture every follicle. The fluids aspirated from the follicles contain the oocytes, which can later be fertilised in the in vitro laboratory. After the procedure, the patient rests for a while and then is discharged and able to resume everyday tasks on that very same day.
The next step is the oocyte in vitro fertilisation, with donor or partner´s sperm. There are two different techniques to carry out the procedure: conventional IVF, during which each and every retrieved egg is placed in previously manipulated sperm in a culture plate, simulating the process of natural fertilisation; and intracytoplasmic sperm injection (ICSI). The second is a high-precision technique, which involves our embryologists selecting the best sperm cells individually and microinjecting them one by one directly into every egg.
If she wishes, the patient may return to her country during embryo culture, which lasts between 5 and 6 days. Our embryologists are in charge of creating stage-specific culture conditions necessary for the embryos, and simultaneously, they observe and analyse their development to assess their quality. What is more, thanks to time-lapse technology, it is possible to monitor comprehensively and in real time, which not only enables assessing the quality in terms of morphological criteria, but also taking into consideration other parameters related to their viability and times of division. This way, we gather valuable, extra information used to discard the embryos that do not evolve correctly and thus, are not likely to result in a pregnancy.
To perform the transfer, the uterus of the patient must be previously prepared, ensuring that the endometrium (the inner layer of the uterus) has the right thickness to receive the embryo and facilitate getting pregnant. During the transfer, carried out at the same IVI clinic where the retrieval took place, the best embryo is introduced into the uterus with the help of a cannula. The procedure takes place in an operating theatre, but it is quick and painless. It is an outpatient treatment, which does not require any type of anaesthesia.
At the same time, the rest of the good-quality embryos not used for the transfer undergo the process of vitrification (cryopreservation), so that they can be employed in a later cycle without the need for further ovarian stimulation.
Once back home, our IVI specialist will tell you the optimum date to take a blood pregnancy test, which is normally 11 days after the transfer. You may resume normal activities as you wait, although it is advisable to avoid the high-intensity ones. If the result is positive, 20 days later your gynaecologist will perform a control ultrasound scan and IVI will then discharge you and you may go on to monitor the pregnancy with your doctor or midwife.