
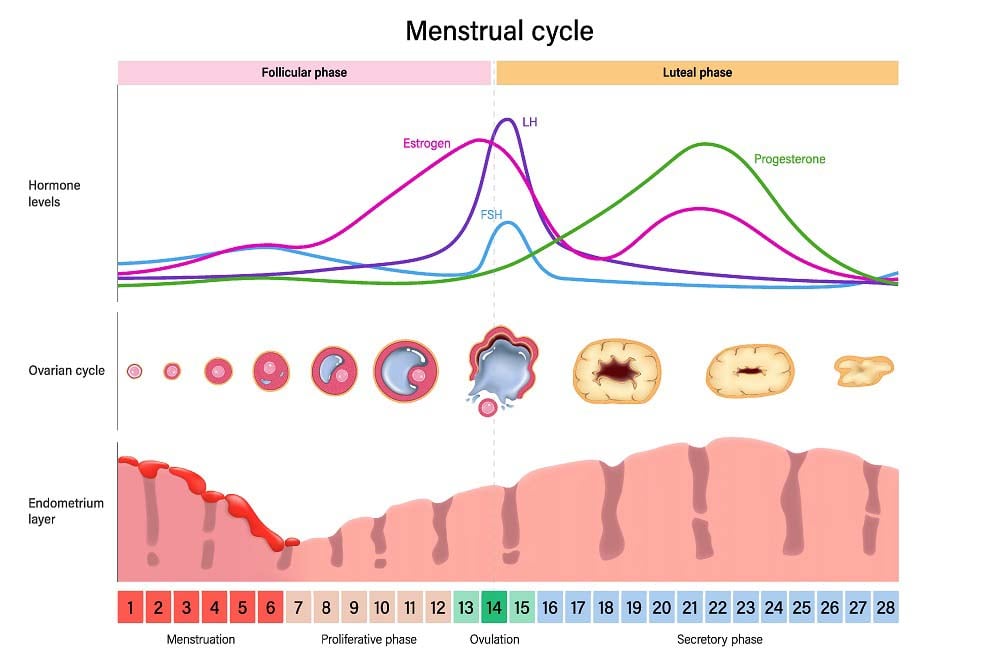
How do hormones control the menstrual cycle? The menstrual cycle is regulated by an interaction between reproductive hormones: LH, FSH, estradiol, and progesterone. This process results in follicular growth, ovulation, and the formation of the corpus luteum. If there is no pregnancy, the decrease in progesterone levels leads to the shedding of the endometrial lining and the restart of the cycle every month.
Today we will talk about how hormones control the menstrual cycle: we’ll give you information about these hormones and their function. What are the typical hormonal changes during the cycle?
What are the 4 main hormones in the female menstrual cycle?
The menstrual cycle has an approximate duration of 28 days from the first day of bleeding to the first day of bleeding of the next cycle. This period can vary and range between 21 and 35 days. Irregularity in menstrual cycles is known as oligomenorrhea, and the complete absence of menstruation is known as amenorrhea.
The menstrual cycle is controlled by four hormones that interact with each other. They are as follows:
- FSH hormone, which contributes to egg production and follicular growth.
- Estradiol, which acts on the dominant follicle.
- LH hormone, which regulates the cycle itself and ovulation.
- Progesterone, which has an effect on the endometrium, preparing it for embryo implantation.
Next, we will see in more detail how these hormonal changes occur during the menstrual cycle.
How do hormones control the menstrual cycle?
Let’s now look at the different stages of the menstrual cycle, which are determined by the interaction of hormones.
Follicular Phase
At the beginning of the cycle, there is a slight increase in FSH hormone levels, which stimulate follicular growth in the ovary. The first part of the menstrual cycle is mainly focused on follicular growth and the selection of a single dominant follicle. That’s why this initial stage is known as the follicular phase.
FSH Window Stage
As the follicles grow, they produce estradiol and inhibin B. Inhibin and decreased levels of estradiol exert negative feedback on the hypothalamic-pituitary-gonadal axis. This leads to a decrease in FSH levels, contributing to the selection of the dominant follicle. This is possible because larger follicles require less FSH to grow, while smaller ones are delayed because they need sustained hormone release. This period is known as the FSH window and leads to the selection of the dominant follicle.
As the dominant follicle continues to grow, it continues to synthesize estradiol. As estradiol levels increase, there is a shift in feedback mechanisms from negative to positive, resulting in an increase in LH levels.
Ovulation and Luteal Phase
The mid-cycle surge in LH levels, lasting 36-48 hours, triggers ovulation or the release of the mature oocyte from the follicle. The remaining follicle forms what is known as the “corpus luteum.” This structure secretes progesterone, reaching its peak levels in the last 14 days of the cycle. This constitutes the luteal phase. The presence of elevated progesterone levels in the middle of this phase indicates that ovulation has occurred.
End of the Cycle
Progesterone prepares the endometrium for embryo implantation if fertilization of the oocyte has occurred. The presence of an embryo induces the secretion of hCG hormone, which helps maintain the function of the corpus luteum. This allows it to continue producing progesterone and sustain the pregnancy.
If fertilization and embryo implantation do not occur, the corpus luteum will regress, leading to a decrease in progesterone levels. This drop in progesterone concentrations leads to the shedding of the endometrial lining and menstrual bleeding, marking the start of a new cycle.
Hormone levels during the menstrual cycle
To measure hormone levels, a test called hormonal determination is conducted. The results of this test can vary depending on age, sex, or health history. The specific laboratory where the test is performed can also influence the results.
FSH Levels
FSH hormone levels are measured in mIU/mL (milli-international units per milliliter). In the case of women, the results can vary depending on the phase of the menstrual cycle. Additionally, there are numerous factors that can cause FSH levels to be either too high or too low. The normal results are as follows:
| Phase | FSH Levels (mIU/mL) |
|---|---|
| Follicular phase | 4–9.9 |
| Ovulatory phase (LH peak) | 2–17.2 |
| Luteal phase | 1–9.2 |
| Postmenopause | 3–100.6 |
LH Levels
Regarding LH, the normal ranges are as follows:
| Phase | LH Levels (mIU/mL) |
|---|---|
| Follicular phase | 68–15.0 |
| Ovulatory phase (LH peak) | 9–56.6 |
| Luteal phase | 61–16.3 |
| Menopause | 2–52.3 |
Abnormally high levels of LH during non-ovulatory periods could be indicative of menopause. They can also reveal polycystic ovary syndrome, a pituitary disorder, nutritional issues, or a stressful situation.
Estradiol Levels
Normal estradiol levels can vary significantly depending on the time period considered. In a normal menstrual cycle, estradiol levels fluctuate as follows:
| Cycle Stage | Estradiol Levels (pg/mL) |
|---|---|
| Menstrual period | < 50 |
| Follicular development | Up to 200 (maximum) |
| Pre-ovulation | Up to 400 (maximum) |
The concentration briefly drops during ovulation and rises again during the luteal phase.
In the absence of pregnancy, estradiol levels decrease to their minimum concentrations at the end of the luteal phase.
If there is pregnancy, estradiol levels steadily increase until the fetus is fully mature. This estradiol comes from the placenta.
Progesterone Levels
Progesterone levels are measured in nanograms per milliliter (ng/mL). The normal levels are as follows:
| Stage | Progesterone Levels (ng/mL) |
|---|---|
| Prepubertal girls | Up to 0.3 |
| Follicular phase | Up to 0.7 |
| Luteal phase | Up to 25 |
| Pregnancy – First trimester | 10–44 |
| Pregnancy – Second trimester | 5–82.5 |
| Pregnancy – Third trimester | 65–290 |
Frequently Asked Questions About Hormones and Fertility
Hormone-related topics often raise many questions. Below, we answer some of the most common ones.
How long is luteal phase?
In most cases, the luteal phase lasts between 10 and 16 days, with 14 days being considered normal. A luteal phase is considered long when high progesterone levels are maintained for more than 16 days after ovulation. Likewise, a luteal phase lasting 10 days or fewer is considered short.
When does LH peak?
LH typically peaks 24 to 36 hours before ovulation. In fact, this peak marks the moment just before the follicle ruptures and releases the mature oocyte. Ovulation itself usually occurs between days 14 and 28 of a normal menstrual cycle.
What does low progesterone mean?
Low progesterone indicates that the ovaries are not producing enough of this hormone, which is essential for preparing the endometrium for pregnancy. Low progesterone levels may be associated with ovulation disorders or a lack of ovulation, as well as a short luteal phase.
What happens to the menstrual cycle when hormone levels are unbalanced?
Unbalanced hormone levels can lead to irregular menstrual cycles, including very long or very short periods, or the absence of menstrual bleeding (amenorrhea).
Consultation with an IVI specialist
Despite the information provided by measurements, it is always necessary to consult the results of the analyses with a specialist to establish a diagnosis. If you would like to schedule tests and analyses, consult with an IVI specialist who will advise you regarding any abnormalities in your cycle. We are world leaders in fertility treatments. Call us or leave your information in the contact form, and our team will get in touch with you.





Comments are closed here.