
A low sperm count leading to infertility is an increasingly common condition in the Western world. A recent study led by Dr Ashley Tiegs, IVI fellow, found that the number of men at risk of needing fertility treatment went from 12.4% in 2004 to 21.3% in 2017. It also reported that male infertility now represents around 50% of all the cases treated by fertility clinics. Her team’s findings have given rise to both alarm and speculation about the possible causes. You may not give a second thought to your, or your partner’s, sperm count until the time comes to start a family. Then it becomes crucial.
In this article we examine the possible causes of low sperm count, its signs and symptoms, how it is diagnosed and, most importantly, the steps you may need to take. What are the options for low sperm count treatment to help you rescue your dreams of having your own family?
Symptoms of low sperm count
The only real symptom of having a low sperm count is infertility. Therefore until you are actively trying to conceive a child, it’s quite likely you will have no idea that there is a problem. However a low sperm count could be associated with other underlying medical conditions, which do have a range of symptoms.
Medical causes of low sperm count
- Varicocele, which is a swelling of the veins that drain the testicles. This is a common cause of male infertility.
- Infections such as inflammation of the epididymis or testicles, or some sexually transmitted diseases can cause scarring that blocks the passage of sperm.
- Ejaculation problems can be caused by health conditions such as diabetes, injuries to the spine or surgery. Some medications such as alpha blockers can also cause ejaculation problems.
- Structural problems such as undescended testicles, genetic abnormalities or a hormone imbalance can also reduce fertility.
If you have any symptoms such as low sex drive, erectile dysfunction or pain and swelling in the testicle area, you should consult your medical practitioner. If you don’t have symptoms but have been trying for a pregnancy for a year without success, it’s time for some diagnostic fertility tests.
Other causes of low sperm count
Even for people who do not have any of these underlying medical conditions, a low sperm count can still be the result of lifestyle and environmental factors. Contrary to popular myth, masturbation is not one of them, and has no impact on the health of sperm.
Lifestyle causes of low sperm count
Heavy use of recreational drugs such as alcohol, tobacco, marijuana, opioids and even use of anabolic steroids for body-building purposes can all have an adverse impact on sperm quality. Long-term mental health issues such as depression or anxiety can also lower sperm count. Maintaining a healthy weight is also important, as being overweight can affect the hormone balance and damage the quality and quantity of sperm.
Environmental factors
The reason that sperm are stored outside the body cavity is that their ideal temperature is slightly below that of the normal body. Anything that heats up the groin area, such as working for long periods with a laptop on your lap or taking long soaks in a hot tub, is therefore not good news for sperm. You should also try to avoid pollutants such as herbicides, pesticides, industrial chemicals and solvents in order to protect your sperm health. This risk is due to working with them or because some of them can be present in the food.
How is low sperm count diagnosed?
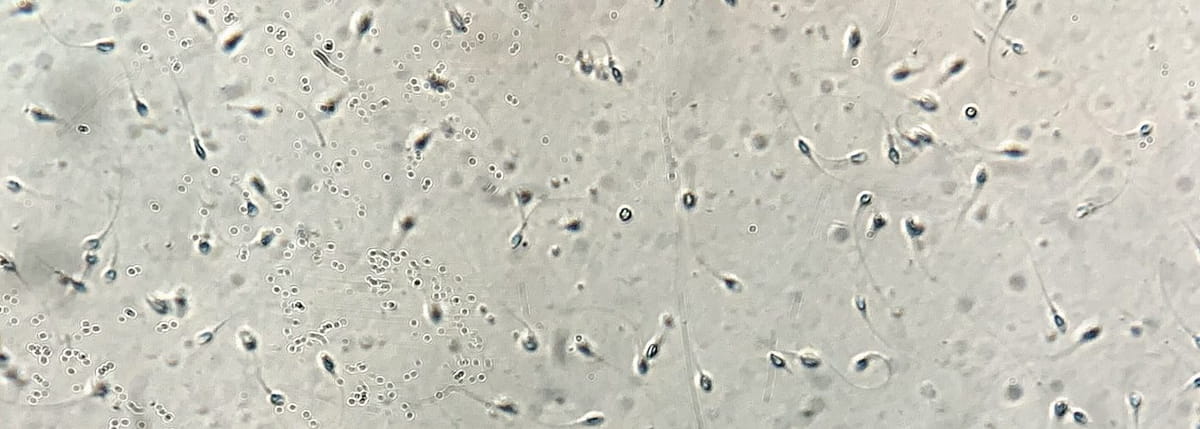
There’s really no other way except for a full semen analysis to diagnose any problem with your sperm count. While it is possible to use an over-the-counter home semen analysis kit, many of these only measure the number of sperm, and quantity is by no means the whole story. A full semen analysis will also examine sperm motility, that is how many of your sperm are capable of swimming, and morphology, the structure and shape of your sperm, as well as acidity, concentration and volume.
A fertility specialist or an assisted reproduction clinic will supplement these technical aspects of semen analysis by taking your medical history and performing a full physical examination. Where necessary, a diagnosis can also include blood tests to check hormone levels, an ultrasound scan of the testicles and prostate and, in the case of blockages, a biopsy to evaluate sperm production.
Fertility treatment for low sperm count
For some of the medical causes of low sperm count, surgery would be needed. Or, in the case of a blockage preventing sperm from entering the ejaculate, a biopsy or just an epididymal aspiration to recover sperm may be necessary. But the good news is that most cases are treatable in terms of fertility. The most commonly used assisted reproduction treatments would be intrauterine insemination (IUI) or in vitro fertilisation (IVF).
Also known as artificial insemination, IUI is recommended for heterosexual couples where the male partner has mild or moderate deficiencies in sperm quality. It increases the chances of pregnancy in three ways:
- The semen sample is prepared in the andrology laboratory to eliminate those sperm which are immobile or slow and select and concentrate only the healthiest.
- Ovarian stimulation may be used to ensure the presence of one or two eggs at the time of ovulation.
- At the right time, the prepared sample is inserted directly into the woman’s uterus, bypassing any possible hostile environment in the vagina, thus maximising the likelihood of natural conception.
The more invasive and complicated but overall more successful technique of IVF may be used when IUI is unsuccessful, and in cases of moderate or severe male factor infertility. This well-known process involves a few more stages than IUI.
- First, ovarian stimulation with hormonal medication ensures the production of multiple eggs. These are collected directly from the follicles in the ovaries in a simple 20-minute procedure carried out under anaesthetic.
- These are then fertilised in the laboratory using sperm which have been prepared in advance, either through mixing with the eggs or through the ICSI technique.
- The resulting embryos are observed and, where necessary, genetically tested as they develop in the laboratory.
- At the appropriate stage of development, a single selected embryo is transferred to the woman’s uterus where, all being well, it will implant and pregnancy will result.
Getting in touch with IVI
A low sperm count doesn’t necessarily mean that you and your partner will not become parents! If you would like to discuss diagnostic testing, or you want to know more about the options for fertility treatment, do get in touch with us at IVI.




Comments are closed here.