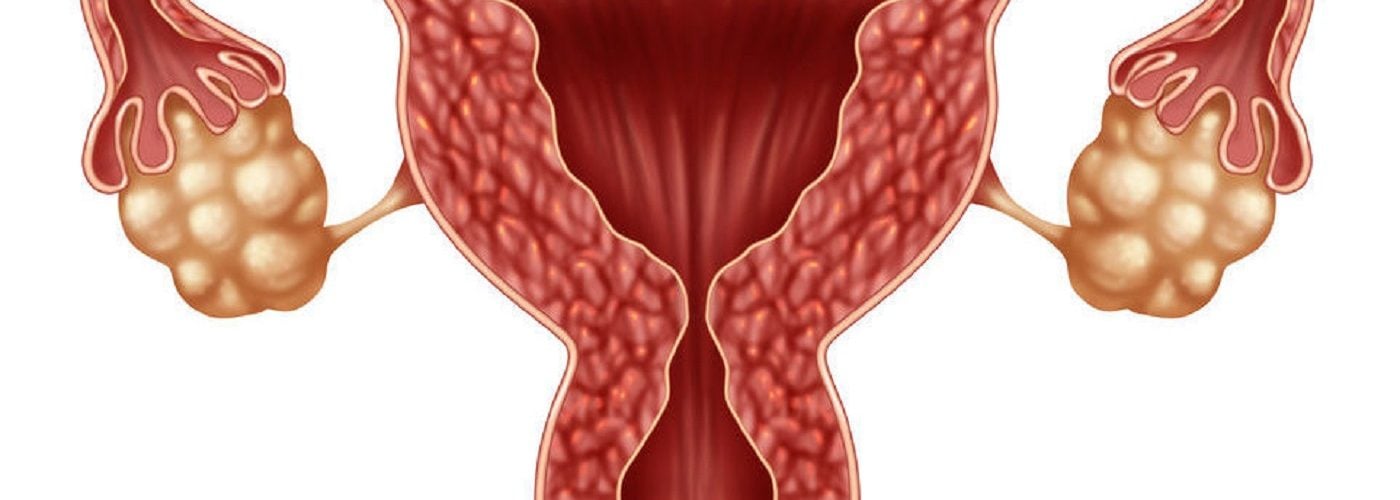
Each ovary contains a variable number of ovarian follicles, and every one of those follicles contains one immature egg, or oocyte. Among all the follicles with oocytes growing inside, only one or maybe two will grow and develop completely, maturing and being released as an egg during the process called ovulation.
Although an ovarian follicle is not a cyst, in some circumstances it can develop into one. So, a follicle is not a cyst, a cyst is not a follicle but it can derive from one, and can occur singly or in multiple form. Confusing? It doesn’t need to be!
In this IVI blog article we aim to disentangle any misunderstandings surrounding the concepts of ovarian follicles and ovarian cysts and clarify the links between the two. To start at the very beginning, we have all heard of a hair follicle, but what is a follicle in ovary terms?
What is an ovarian follicle?
Even before a girl is born, while she is still in the foetal development stage, her ovaries contain primordial follicles. These remain in an undeveloped ‘sleeping’ state until she reaches puberty. Before birth, the two ovaries contain anything from 600,000 to 1,000,000 follicles. Fewer than 1% of these will ever reach maturity. Starting at puberty, a few of these primordial follicles become primary follicles in a process which goes on every day until menopause. Some of these develop through the secondary and then antral follicle stages, at which point they are large enough to be detected by an ultrasound scan. Only one or two in each monthly cycle eventually become large enough to produce a mature egg. After releasing the single egg that it contains during ovulation, the empty follicle becomes what is known as a corpus luteum.
The follicles are not merely passive little packages patiently waiting their turn to produce an egg. They play a very active and essential role in the whole menstrual cycle. They protect and nourish the oocyte as it develops into a mature egg and interact with the pituitary gland to regulate the hormone balance that eventually leads to the complete maturing of an egg, and ovulation. Even after releasing the egg, the follicle – now a corpus luteum – continues to play a role in the production of progesterone and oestrogen, which are crucial to sustain the pregnancy and the development of the foetus and the placenta.
When and why does a follicle become a cyst?
Sometimes a hormonal imbalance can prevent developing follicles from reaching maturity and releasing an egg. Most follicles containing an egg that fails to mature disintegrate naturally in a process known as atresia. But occasionally, the follicle accumulates fluid or blood and develops into a cyst. Most of these are completely harmless and resolve themselves within a matter of months; in fact, many women would not know they had an ovarian cyst unless it was discovered during a routine pelvic examination. The single cyst or multiple ovarian cysts do not normally cause any significant problems or have any impact on fertility. In a minority of cases, however, problems can arise.
If you were to develop an ovarian cyst that became so large it caused pain or blocked the ovaries or fallopian tubes, it may need surgical treatment. Multiple cysts on the ovaries, known as polycystic ovaries, can be part of a condition known as polycystic ovary syndrome (PCOS). Like all syndromes, this is a collection of symptoms which can include a hormone imbalance and irregular or absent ovulation as well as the characteristic multiple cysts. In cases where PCOS causes irregular or absent ovulation, this will clearly lead to fertility problems, and in fact PCOS is one of the main causes of infertility in women.
What is the fertility treatment for PCOS?
The specific fertility treatment recommended if you have PCOS is a matter for your fertility specialist and will depend on your individual circumstances. However, it is quite possible that if you have ovulation problems resulting from PCOS, they will be solved by using oral contraceptive pills, which may balance again your hormone levels. If that´s not the case, your recommended treatment will be either intrauterine insemination (IUI) or, if this is unsuccessful or inappropriate in your case, in vitro fertilisation (IVF). In both cases, this brings us back to the follicles. For both of these treatments it is important that you have an adequate number of follicles able to produce the optimum number of eggs, but the optimum number is very different in each treatment.
Intrauterine insemination fertility treatment
In IUI treatment, hormonal fertility drugs are used to stimulate the follicles in the ovaries to produce one, or at most two mature eggs. This is because the treatment involves inserting a prepared sperm sample directly into the uterus at the time of ovulation in order to maximise the chances of conception. If there were more mature eggs than the optimum number, there would be the danger of a multiple pregnancy, which brings serious health risks to both mother and children. Therefore, for an IUI patent, less is more: the quality of the egg is the important issue, and one follicle producing one good egg is all you need.
In vitro fertilisation fertility treatment
For an IVF patient on the other hand, the number of follicles producing mature eggs could be seen as the more the better. IVF patients will probably have had their ovarian reserve, that is the estimated number of follicles in the ovaries, tested during the initial stages of fertility investigations. Once the course of IVF treatment starts, the growth and development of the follicles is closely monitored through ultrasound scans. The amount of oestradiol in the blood is also monitored as the level of this oestrogen, produced by the developing follicles, is a good indicator of their health and normal development.
When the follicles are at the right stage of development, a hormone injection triggers the final maturing of the eggs so that they can be retrieved. Since fertilisation then takes place in the laboratory, the risk of multiple pregnancy is removed, and the single healthiest embryo can be selected for transfer to the uterus.
Contacting us at IVI
It’s all very well to have any confusion between follicles and cysts cleared up but for women concerned about their fertility, this may not be all that’s needed. If you want practical assistance as well as clarification, do get in touch. Although there are no guarantees, there is a very good chance that we can help. Have a look at our IVF success rates, or just use our online contact form to ask a question or make your first appointment with IVI.




Comments are closed here.