
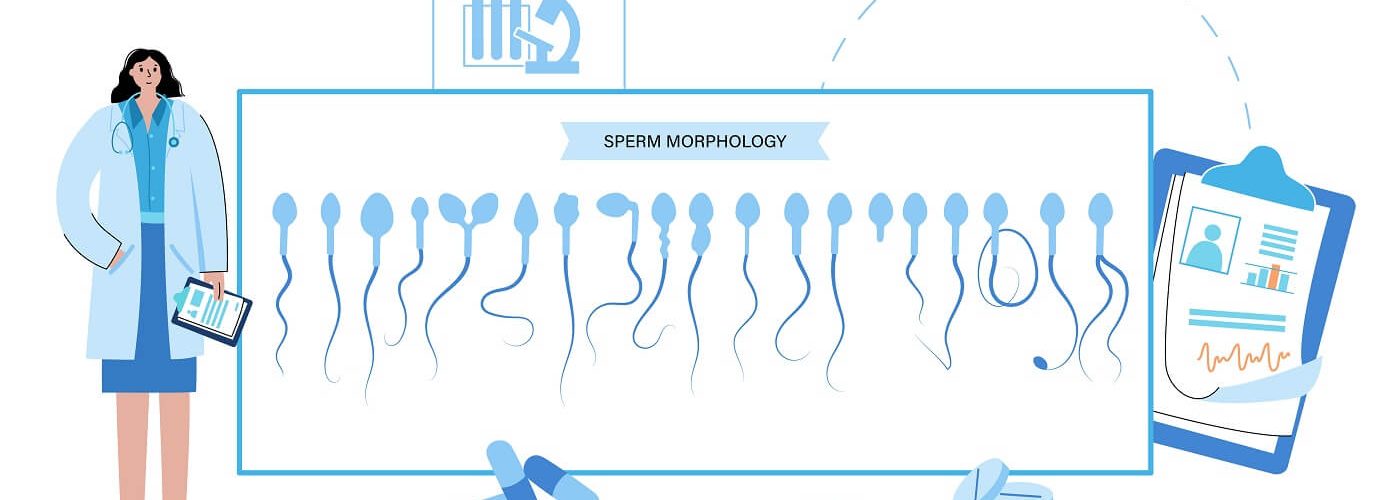
Sperm morphology is one of the parameters analyzed in a semen analysis to assess the state of male fertility. Studying sperm morphology involves analyzing the shape and size of spermatozoa. This article delves into what sperm morphology means, what the normal values are, what possible causes for abnormal values exist, and the available treatment options available.
What is morphology in sperm
As mentioned before, sperm morphology encompasses the shape and size of spermatozoa. Evaluating it helps determine the quantity of spermatozoa with abnormalities and the underlying causes. All men have spermatozoa with abnormal morphology. The World Health Organization (WHO) states that 4% of spermatozoa analyzed in a sample should exhibit normal morphology. If the semen analysis shows lower values, the patient is diagnosed with teratozoospermia.
When is sperm considered to be normal?
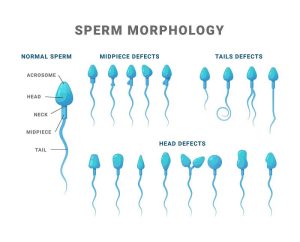
A sperm is considered normal when it exhibits an oval-shaped head, a straight flagellum, and a fixed, transparent nucleus with regular contours. Conversely, a sperm is morphologically abnormal when it presents abnormalities in its head (elongated or too large) or flagellum (double or coiled). Teratozoospermia can manifest in varying degrees, leading to consequences ranging from slowing sperm movement to complete impairment of fertilization capacity.
Causes of abnormal sperm morphology
Several factors contribute to teratozoospermia or the presence of a high percentage of spermatozoa with abnormal morphology. The most common ones include:
- Genetic alterations
- Semen infections
- Testicular infections or injuries
- Varicocele
- Radiation or chemotherapy treatment
- Harmful habits like tobacco or drug use
- Vasectomy
- Diabetes
- Environmental conditions leading to increased testicular temperature
- Correcting Sperm Morphology
How to correct sperm morphology
When a couple struggles to conceive naturally, their lifestyle habits should be the first aspect to examine. Regular exercise, a healthy diet, avoiding nicotine and alcohol when possible, and reducing stress can improve sperm quality and quantity. Additionally, specific supplements can be included in the diet to promote male fertility, such as omega-3 fatty acids, antioxidants, L-carnitine, and vitamin E. Exercise can also boost testosterone levels.
Often, a seminal pathology like teratozoospermia necessitates assisted reproduction techniques, such as in vitro fertilization (IVF). If spermatozoa are fertile, testicular sperm extraction may be possible. This involves extracting spermatozoa from testicular tissue through a testicular biopsy. The success rates of this method increase further with new procedures for selecting mature spermatozoa and separating less suitable ones, known as Intracytoplasmic Morphologically Selected Sperm Injection (IMSI).
Sperm selected through this method is utilized by the physician as part of artificial insemination treatment. Possible procedures include:
- In Vitro Fertilization (IVF)
- Artificial Insemination
- Intracytoplasmic Sperm Injection (ICSI), a technique within IVF where spermatozoa are injected directly into the egg cytoplasm under a microscope.
If these procedures are not suitable or successful, assisted reproduction through sperm donation may also be a solution to fulfill the desire for children in cases of male infertility.
Other male infertility issues
Teratozoospermia is not the only male infertility problem detectable in a semen analysis. Besides sperm morphology, parameters studied in this test include:
- Ejaculate volume
- Concentration (million spz/ml)
- Level of sperm motility
Oligospermia
Occurs when the semen analysis shows a low sperm count in the analyzed sample. The WHO sets normal values at < 15 million/ml or < 39 million per ejaculate. Oligospermia can be mild, moderate, or severe.
Azoospermia
Observed when there is a total absence of spermatozoa in the semen analysis. The cause may be the inability to produce sperm or obstruction of the transporting ducts.
Astenozoospermia
When the semen analysis indicates that less than 40% of spermatozoa have a normal mobility.
Necrospermia
Occurs when less than 54% of observed spermatozoa are alive. It can be total or partial and may result from genital tract infections, trauma, medical treatment, or genetic alterations, among other causes.



Comments are closed here.