- Preimplantation genetic testing and the specialisation of the embryologist provide safety and confidence for the success of reproductive treatments.
- Assisted reproduction processes do not have a negative impact on patients who have previously had a COVID-19 infection.
The 77th edition of the Congress of the American Society for Reproductive Medicine (ASRM), one of the most important Assisted Reproduction encounters in the world, has just come to an end. This year it was held in virtual format once again due to the health situation, and researchers and specialists in Reproductive Medicine met to share the latest findings in the reproductive field.
This year, IVI presented nearly 70 papers, all of them focused on offering the greatest safety and the best guarantees to the women and couples who entrust them with their desire to get pregnant.
“There are many lines of research that shape our daily work, always under the premise of offering the best results to our patients and making their experience as bearable as possible. Our priority is to ensure that they achieve their baby in the shortest time and with the best guarantees, taking care of every step of the process. Our firm commitment to research and our participation in leading congresses such as this one help us to continue leading this constantly evolving field”, said Dr. Nicolás Garrido, Director of the IVI Foundation.
PGT-A and the work of the embryologist: keys to treatment success
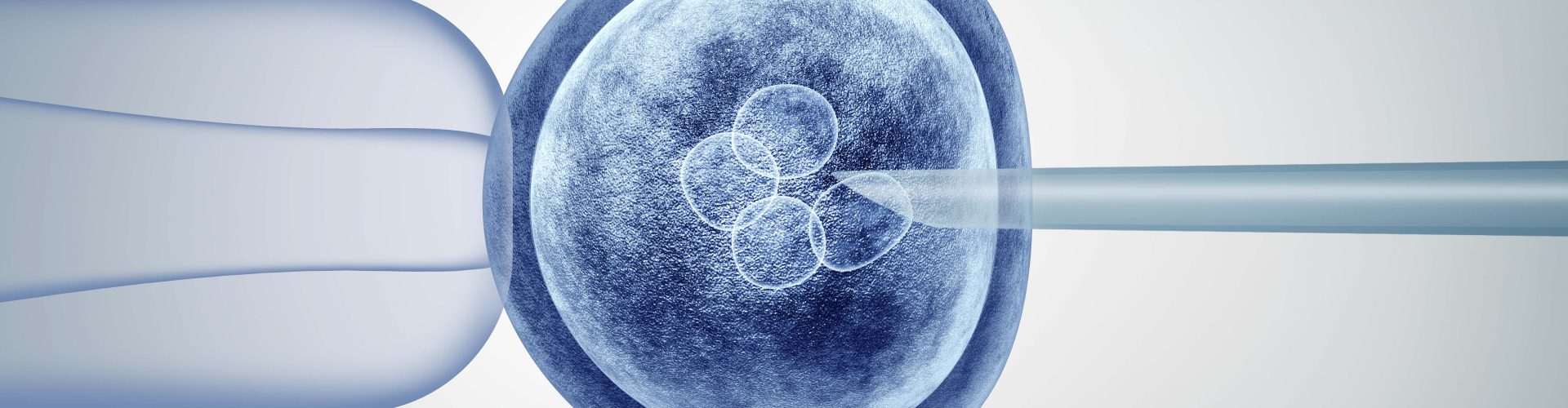
The embryologist’s role is key in an assisted reproduction process, as their criteria is fundamental when selecting the best embryo to transfer. In this sense, to date it has not been analysed whether the morphological classification systems or other subjective strategies used by embryologists help to select euploid embryos –containing 46 normal chromosomes– with greater probability than aneuploid embryos –with an imbalance in chromosome complement.
Fully aware of this reality, IVI has studied how the morphological classification systems used in the embryology laboratory preferentially select euploid embryos.
“Out of a total of 156 single embryo transfers (SET), 129 were euploid, selected by embryologists blinded to the result of the embryo biopsy and subsequent PGT-A (pre-implantation genetic testing performed on the embryo) to determine the embryo typology. This shows that embryologists are highly skilled in selecting euploid embryos to be transferred to the maternal uterus, according to the morphological classification”, explained Dr. Garrido.
Another of the papers presented at the ASRM aims to determine the nature of chromosomal errors in human embryos, and how these anomalies can affect the interpretation of the PGT-A results of the embryo.
“An initial euploid or aneuploid result is reconfirmed in the rest of the embryo in almost all cases, demonstrating how meiotic errors –which take place during cell division– occur in almost the entire embryo. Thus, the observed discordance rate of 2% is consistent with the mosaic rate in the general population, so the combination of a reliable analytical platform and new advances in understanding the biology of embryonic errors should boost confidence in PGT-A results”, said Dr Garrido.
Yes, reproductive treatments are safe after COVID-19
COVID-19 continues to be a hot topic. At this year’s ASRM, IVI also presented results in patients seeking help from reproductive medicine to achieve a baby after COVID-19 infection.
“What is certain is that, in an infertile population, a recent history of COVID-19 diagnosis does not have a negative impact on pregnancy outcome compared to a control population, although the study needs to be expanded to a larger sample. This helps us to reassure patients who are wondering about the safety of reproductive treatments regarding the Coronavirus, urging them not to delay their processes once they have recovered from the disease”, concluded Dr Garrido.
