
- In Fertility Month, IVI shares the pillars on which its success is based
- The cumulative rate after three attempts at in vitro fertilization and egg donation is very close to 100%.
Ensuring patient safety at every step, achieving the impossible, investing in cutting-edge research and learning to control time in order to have the best success rates are the four differentiating elements in offering quality assisted reproduction treatments, which only the best fertility clinics can guarantee.
Fertility month is our month, when we most celebrate the miracle of motherhood, and this year is special because we have reached 30 years of making our patients’ dreams come true. For this reason, we want to tell you what goes into making this miracle.
Safe assisted reproduction
We live in an age of safety, exacerbated by the most lethal pandemic of the 21st century. The return to fertility treatments in clinics has been orchestrated by comprehensive safety measures. More than fifteen measures are included in the safety protocol at all IVI clinics. In addition to the basic measures (gloves, masks, protective screens, hydroalcoholic gel…) all our laboratories have been equipped, for many years, with the necessary processes to work with type 2 infectious agents such as Zika or HIV and, of course, SARS-CoV-2. A this time of uncertainty due to COVID-19, all our patients (both women and men) are subjected, at every step of the assisted reproduction process, to diagnostic tests to rule out the presence of Coronavirus and check whether they have immunity or not.
Obtaining a healthy baby and the mother’s safety throughout the treatment are IVI’s maxims. Safety that is summarized by the two current popular acronyms SET (single embryo transfer) and PGT (preimplantation genetic testing). Ensuring equal or greater success rates with single embryo transfer is something that only the most specialized clinics can offer. IVI has reduced the rate of twin pregnancies by 75% in the last ten years, due to the risks (prematurity, low birth weight, hypertension…) that these entail. And our commitment to the safety of our patients and their babies has increased our SET rates to 84.8% per cycle in IVF and 88.2% in egg donation.
Also increasing the rate of preimplantation genetic testing, for the detection of genetic and chromosomal abnormalities and the prevention of transmission of serious diseases, and obtaining a cumulative pregnancy rate of up to 73.4%.
You can see more advantages of single embryo transfer in this video:
We could not close the chapter on safety without mentioning the Matcher, the barcode and scanner system guaranteeing the correct traceability of all our samples (at all our centres) and the screening test for monogenic diseases that we apply to all our donors, which is essential to ensure the absence of genetic risk in gamete recipients.
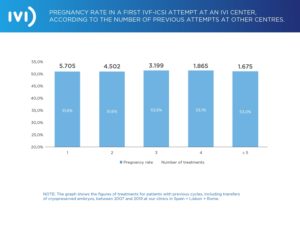
Complicated medical cases at IVI
Achieving the impossible is not a pipe-dream when we look at our pregnancy rate (see graph below), regardless of the number of previous treatments a patient has undergone before coming to our clinics. From one to five or more previous attempts, we find an average pregnancy rate of over 50%. This means that, regardless of the previous history and the complexity of the previous treatments, we will ensure our patients get pregnant.
Did you know that IVI was one of the pioneering clinics in having its data audited by a third party? Did you know that all IVI data is validated annually by SGS, the world leader in inspection, verification, testing and certification? This allows us to be extremely precise when comparing our data with that of the SEF (Spanish Fertility Society), and in that comparison we extract very conclusive data, such as the fact that our rate of implantation with own oocytes is almost double the national average in most Autonomous Communities and the gestation rate is around 15% higher than the average.
Helping our patients to achieve their dream of becoming mothers, regardless of their history of previous treatments, or the complexity of their case, is close to achieving the impossible. We know how long and difficult the road to motherhood can be at times, which is why we collaborate with all our patients to improve the emotional and economical aspects by making their dream of becoming mothers come true in the shortest possible time.
Research and success rates at IVI
More than 1,900 researchers, 28 laboratories in 9 countries, 15 lines of research, around 150 publications per year, with only one goal: our patients. Research is our driving force; we could not guarantee safety standards or dream of achieving the impossible without leading research in the field of reproductive medicine. ESHRE, the highest authority in Europe, and probably in world, on human reproduction and embryology, will soon hold its congress, an event we will attend as the largest group worldwide in terms of the total number of papers presented and approved, with a total of 52.
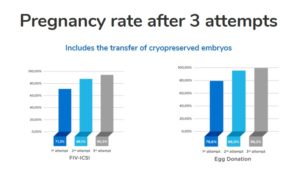
Our studies, our research, are the key to increasing and guaranteeing our success rates year after year. This way, in both IVF and egg donation our success rates are around 70% and 80% in a single attempt, while the cumulative rate after three attempts in both cases is very close to 100%.
Time and age in assisted reproduction
Far from the romantic idea of holding back time, many of the advances in assisted reproduction allow us to control it. Starting with the AMH (anti-Müllerian hormone) test, which is a blood test that gives us the ovarian reserve in order to assess whether it is time to consider motherhood. And if the biological clock is ticking but the second hand of the socio-economic and emotional clock is behind, it is time to consider preserving fertility or vitrification of oocytes, the female revolution of this century. The possibility of preserving one’s own gametes in order to decide to use them when the biological, socio-economic and emotional clocks converge.
Aside from the most well-known options, IVI wages its own particular battle against time with several studies currently underway on the concept of ovarian rejuvenation. The first, with a longer history and several babies born thanks to this technique, consists of regenerating the ovarian niche by infusing platelet-rich plasma from stem-cell-rich blood. The stem cells provide the factors that regenerate the ovarian niche so that the existing follicles in the ovary can be activated for their growth and maturation.
Another more recent line of research is working on trying to recover (lengthen) the telomeres (ends of the chromosomes, indicators of ageing) by means of a specific medication. In other words, research is being carried out to prevent the progressive deterioration of the telomeres in those patients with specific pathologies, for example low ovarian reserve, i.e. with ageing ovaries.
All of the above can be summed up in the passion the medical team at IVI clinics has for science, research and life, and all to help couples and/or women who want to have a child.




Comments are closed here.