The septate uterus is one of the most common uterine malformations. Although it is often asymptomatic, it does pose a problem for women seeking pregnancy, as it can affect their fertility.
Today, we will discuss this condition, how to detect it, how to treat it, and what alternatives are available when it impacts the goal of starting a family.
What is a septate uterus?
A septate uterus is a uterus which is divided into two by a septum. This word comes from septum, which is simply a tissue dividing two chambers, such as those found in the heart or the middle of the nose.
Although the condition is not in itself damaging or dangerous, it can have an impact on pregnancy. It is known to increase the risk of miscarriage. Diagnosis often does not take place until after a miscarriage, but once detected, treatment is relatively straightforward.
Types
We can differentiate three types of septate uterus:
- Partial septate uterus, if the septum doesn’t include the cervix.
- Complete septate uterus, when the cervix is also included, which is the opening of the womb.
- Septate uterus and vagina.
How common is a septate uterus?
This malformation of the uterus is believed to be the most common of uterine abnormalities. It affects 1% women. Indeed, it is so frequent that some authorities consider it a variant of normality.
Symptoms of a septate uterus
Most cases of septate uterus are asymptomatic. However, they are occasionally characterized by these effects:
- Dysmenorrhea: pain during menstruation and other discomforts such as cramps or dizziness.
- Spontaneous abortions, before week 20.
- Premature birth or abnormal foetal positions that can make natural childbirth difficult.
What causes a septate uterus?
A septate uterus is a congenital condition. This means that it occurred during the development of the female foetus in the womb before birth. It is not clearly understood why it happens. In the female foetus, the uterus starts out as two tubes that eventually fuse together to form one chamber in the body’s mid-line.
The extent of the septum varies between individuals in a wide range from a minimum to practically complete. This creates a complete separation between the two cavities. This is known as a double uterus.
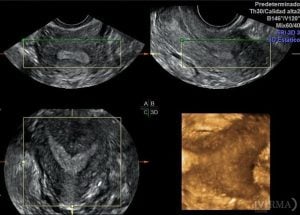
How is a septate uterus diagnosed?
A septate uterus could be detected as a result of a routine ultrasound or MRI (magnetic resonance imaging) scan, but this is not always the case. There are more reliable tests to diagnose this abnormality:
- Hysteroscopy, in which the interior of the uterus is visually examined with the help of an illuminated medical instrument.
- Hysterosalpingogram, in which liquid is inserted through the cervix into the uterus and fallopian tubes. This is the most reliable diagnostic method. The liquid contains a dye which shows up on an x-ray, allowing the examiner to see the shape of the organs on a screen.
Treatment for septate uterus
The main treatment is removing the septum with a relatively straightforward surgical process, depending on its size. The uterus is enlarged with a fluid and then a small surgical instrument is inserted through the vagina to trim away the septum. This hysteroscopic surgery is performed under sedation and takes approximately 15 to 20 minutes.
After removal, when the uterus has healed, it provides the normal environment in which a foetus can implant and develop. For the healing to take place before pregnancy, doctors usually advise a period of two or three menstrual cycles before trying to get pregnant.
How to prevent a septate uterus?
There is some comfort in the fact that a congenital condition is only rarely due to genetic factors. In most cases, if you did find that you had a septate uterus, you would only have your own condition to deal with and would not have the additional worry of passing it on to future generations of daughters. You would also have no need to be concerned about the condition at all if you did not want to have children since in itself it poses no health threat or increased risk of cancer or any other disease. It is only a problem for women who do wish to have children.
However, as it has a congenital original, there is nothing that can be done to prevent a septate uterus.
How does a septate uterus affect pregnancy?
A septate uterus has no effect on a woman’s ability to conceive. Rather, it can have consequences on the development of pregnancy. We will address the main concerns of patients with this condition below.
Do I have a higher risk of miscarriage?
A septate uterus does increase the likelihood of a miscarriage and could well be a factor in cases of recurrent miscarriage. This is frequently since the septum itself has a poor blood supply. So, if an embryo were to implant on the septum, it would be unable to develop in the normal way since the source of sustenance is cut off.
There are no hard and fast statistics on the extent of the risk because it is not always possible to pinpoint the cause of a miscarriage and having a septate uterus does not always, or inevitably, lead to miscarriage. However, it is estimated that the likelihood of miscarriage with this condition is between 25% and 47%, compared with an overall miscarriage rate of 10% to 25% in the general population. A miscarriage caused by this condition usually occurs during the first trimester because of problems resulting from the embryo implanting on the septum. Miscarriage can also occur during the second trimester when the problem is lack of space for foetal development due to the reduced capacity of the uterine cavity.
Will I have more difficulties to get pregnant?
As mentioned, uterine malformation does not affect a woman’s ability to conceive. It also does not imply a greater difficulty in achieving pregnancy.
Will I have a normal pregnancy?
Even for women who do not miscarry, this condition makes a premature or pre-term birth more likely. In addition, there is frequently a need for delivery by caesarean section because the lack of space caused by the septum means that the baby is unable to get into the correct position for birth.
How can a fertility clinic consultation help? (h3)
Anyone who has experienced the shock and grief of a miscarriage is bound to want to know why, and whether a future occurrence could be prevented. When you make an appointment for an initial consultation at one of our IVI clinics, the consultant will of course ask about your medical history. They will also run several diagnostic tests, which for a woman would include a hysterosalpingogram. This would show if there is any uterine abnormality.
You can find out more about what to expect from your first visit to IVI and gen up on the whole range of tests and treatments available. Or just go ahead and contact us at IVI and we will get right back to you.

Comments are closed here.