
Most of us are well aware of the main steps of the IVF process. In it the patient’s ovaries are stimulated, multiple eggs are collected and then fertilised in the laboratory. The final step is when a selected embryo is transferred to the patient’s uterus. It hopefully implants there and continues to develop into a successful pregnancy. But many people are quite hazy about what happens during the interval between fertilisation and embryo selection for transfer.
In this IVI blog article, we’re putting this short stage of the IVI process, only around five days, under the microscope. How does an egg fertilised in the laboratory develop into an embryo capable of implanting in the womb? How does embryo selection work? Which technology do we use to grade them? What is our way to know which embryos are good? Let’s talk about IVF embryo grading.
Development of the fertilised egg
First of all, let’s see how the embryo starts to develop from the very beginning, day by day.
- When an egg is fertilised by a sperm in the laboratory, or in the human body for that matter, egg and sperm fuse into one single cell known as a zygote. It remains a single cell for about 24 hours.
- Typically, on day 2, the single cell has divided into two or possibly four cells.
- Day 3, and the embryo now has six to eight cells and is known as a multicell embryo.
- During day 4, sometimes known as the day of rest, the cells are undergoing the transition process of compaction. The cells are now closely compacted, forming a morula. Once the morula forms, a cavity forms in the middle, in the process of blastulation.
- By day 5 or 6, the embryo has become a blastocyst. The cells have started to differentiate into the inner cell mass that will become the baby and the outer layer, the trophectoderm, which is destined to form the placenta.
Why do we need to select an embryo?
In the natural process of human reproduction, it’s perfectly normal that not all embryos are capable of healthy development. Those that are not viable would usually result in an early miscarriage. This could be because the embryo has genetic abnormalities or other problems. Naturally, we aim to avoid this in the IVF process. That’s why, since the early days of the technique, embryologists have needed to observe and monitor the fertilised eggs as they develop. Then, at the optimum time for transfer to the uterus, they can select the embryo that looks healthiest and most capable of developing into a successful pregnancy. They do this through IVF embryo grading.
IVF embryo grading
Originally, embryologists used to grade embryos examining their development under a microscope. They making a judgement, based on their visual observation and their accumulated expertise and experience. These days, technology has moved on and grading can be carried out with the aid of new technologies. In either case, embryos are graded at day 3 of their development using a simple tabular system:
Day 3 embryo grading and what it means
The grade is allocated to a particular embryo judging by how it looks. For example, in a grade 1 embryo the cells are of equal size and there is no sign of fragmentation. These are the grades:
- Cells are equal in size and there is no visible fragmentation.
- They are equal in size with only minor fragmentation.
2.5. Cells are mainly equal in size with a moderate level of fragmentation.
- They are not equal in size, fragmentation is none to moderate.
- Cells are equal or unequal in size with moderate to heavy fragmentation.
Day 5 embryo grading
The system used to grade embryos on day 5 of development, when they are becoming blastocysts, is more complex. They are starting to form the Trophectoderm Epithelium (TE), the outer shell which will become the placenta, and the Inner Cell Mass (ICM) which becomes the foetus. Together they form a fluid-filled sphere which is also expanding. These three main aspects of development are graded individually in a number and letter system from A to D which make up the overall ‘score’:
- Number: The stage of expansion the blastocyst has reached.
- First letter: The grade of the ICM.
- Second letter: The grade of the TE.
However, this is not an exact predictor and a high score is not necessarily a guarantee of a successful transfer and pregnancy. It’s possible for an embryo graded as 5AA to be unsuccessful whereas an embryo classified as 4BC may turn out to be successful.
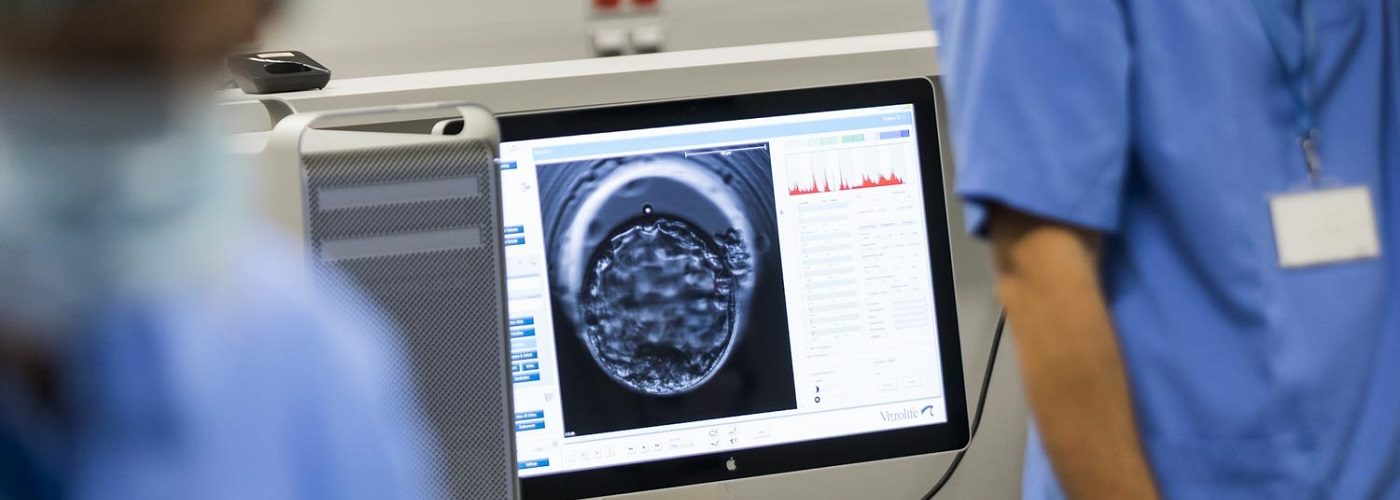
The EmbryoScope: a significant technological advance
The advent of the EmbryoScope incubator has not only replaced, but significantly improved some of these grading processes. Although in the end, we still rely on the skills of experienced embryologists. The EmbryoScope uses time-lapse technology and a sophisticated algorithm, both of which have allowed for significant improvements:
- It maintains constant culture conditions and removes the need for the embryo handling previously necessary to monitor development. This reduces environmental stress on the embryo and results in higher implantation and pregnancy rates.
- It provides vital information not only on the ‘appearance’ of the embryo but also the speed of cell division and the stage it has reached. This information has facilitated the development of mathematical models to judge the viability of the embryo and has enabled a better understanding of the optimum time for embryo transfer.
- It has the added advantage of providing patients with a real-time film record of their future baby from its biological beginnings.
How IVI can help
If you would like to know more, our website has a full description of the IVF process, so you can see where embryo selection fits in to the overall picture. You may also be interested to find out how pre-implantation genetic testing can help even further with embryo selection, when there is a medical need, for example if either prospective parent is in danger of passing on an inheritable condition. To discuss any of these issues with one of our fertility experts, just get in touch using our online contact form.



Comments are closed here.